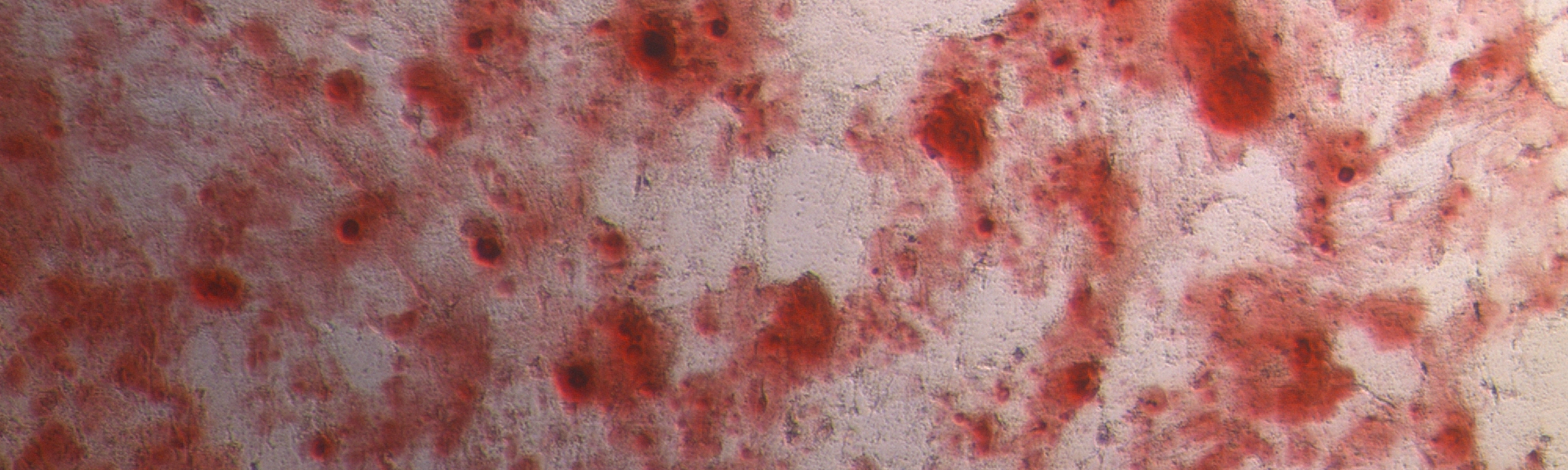
During musculoskeletal surgery, an undefined mixture of bone marrow, cancellous bone fragments, fat, hematoma and additional soluble factors occur at the bony implant site. Together with inflammatory cytokines and nervous stimuli, this microenvironment includes a strong osteogenic potential, associated with an increased risk for ectopic bone formation (non-hereditary heterotopic ossification).
Usually, this “bone stew” is being collected in a plastic-filter of conventional suction handles and later disposed.
Meanwhile, recent research data suggests that the collected surgical-site released tissue is able to enhance local osteoinduction.
These newly identified tissue characteristics were designated “osteopromotive” and led to the BoneFlo®+ Concept.
Ceramic scaffolds in a vacuum suction handle for intraoperative stromal cell enrichment:
The collected surgical-site released tissue in a plastic-filter of conventionel suction sets possesses osteopromotive properties but is usually being disposed. To make this tissue useful for bone regeneration, we developed the BoneFlo®+ Concept.
It is based on the following study which was recently published in International Journal of Molecular Sciences:
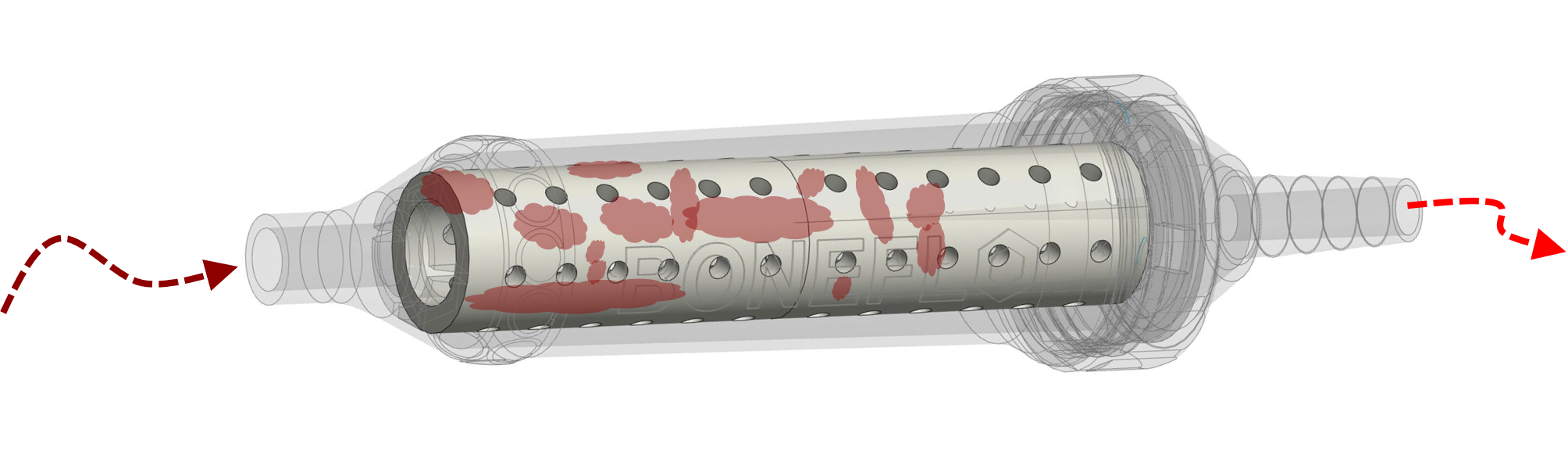
Background: During total joint replacement, high concentrations of mesenchymal stromal cells (MSCs) are released at the implantation site. They can be found in cell–tissue composites (CTC) that are regularly removed by surgical suction. A surgical vacuum suction handle was filled with bone substitute granules, acting as a filter allowing us to harvest CTC. The purpose of this study was to investigate the osteopromotive potential of CTC trapped in the bone substitute filter material during surgical suction.
Methods: In the course of 10 elective total hip and knee replacement surgeries, β-tricalcium-phosphate (TCP) and cancellous allograft (Allo) were enriched with CTC by vacuum suction. Mononuclear cells (MNC) were isolated from the CTC and investigated towards cell proliferation and colony forming unit (CFU) formation. Furthermore, MSC surface markers, trilineage differentiation potential and the presence of defined cytokines were examined.
Results: Comparable amounts of MNC and CFUs were detected in both CTCs and characterized as MSC ‰ of MNC with 9.8 ± 10.7‰ for the TCP and 12.8 ± 10.2‰ for the Allo (p = 0.550). CTCs in both filter materials contain cytokines for stimulation of cell proliferation and differentiation (EGF, PDGF-AA, angiogenin, osteopontin).
Conclusion: CTC trapped in synthetic (TCP) and natural (Allo) bone substitute filters during surgical suction in the course of a joint replacement procedure include relevant numbers of MSCs and cytokines qualified for bone regeneration.
Surgical vacuum filter derived stromal cells are superior in proliferation to bone marrow aspirate:
This study was recently published in Stem Cell Research & Therapy and formed the basis for the BoneFlo®+ Concept.
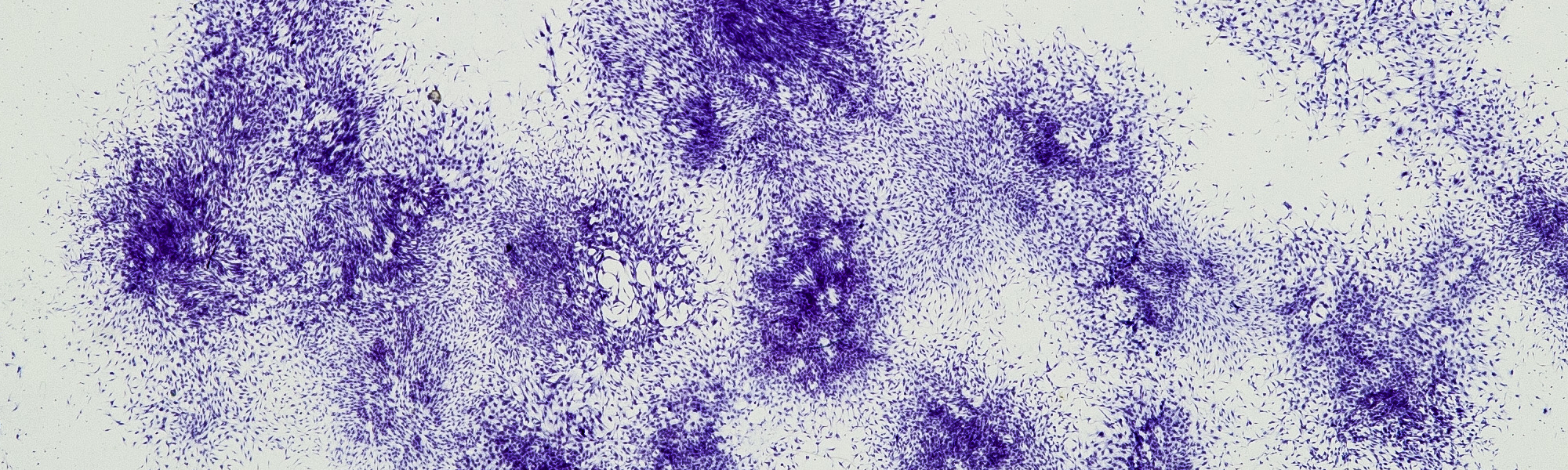
Background: During joint replacement, surgical vacuum suction guarantees a sufficient overview on the situs. We assume high concentrations of mesenchymal stromal cells (MSCs) on surgical vacuum filters. We compared the in-vitro proliferative and differentiation potency of cells from: (i) bone marrow (BM), (ii) cancellous bone (CB), (iii) vacuum filter (VF), (iv) cell saver filtrate reservoir (SF) in 32 patients undergoing elective total hip replacement.
Methods: Mononuclear cells (MNC) were isolated and cell proliferation and cell-forming-units (CFU) were measured. Adherent cells were characterized by flow cytometry for MSC surface markers. Cells were incubated with osteogenic, adipogenic and chondrogenic stimuli. Cells were cytochemically stained and osteoblastic expression (RUNX-2, ALP, and BMP-2) investigated via qPCR.
Results: Dependent on the source, initial MNC amount as well as CFU number was significantly different whereas generation time did not vary significantly. CFU numbers from VF were superior to SR, BM and CB. The resulting amount of MSC from the respective source was highest in the vacuum filter followed by reservoir, aspirate and cancellous bone. Cells from all groups could be differentiated into the three mesenchymal lines demonstrating their stemness nature. However, gene expression of osteoblastic markers did not differ significantly between the groups.
Conclusion: We conclude that surgical vacuum filters are able to concentrate tissue with relevant amounts of MSCs. A new potent source of autologous regeneration material with clinical significance is identified. Further clinical studies have to elucidate the regenerative potential of this material in an autologous setting.